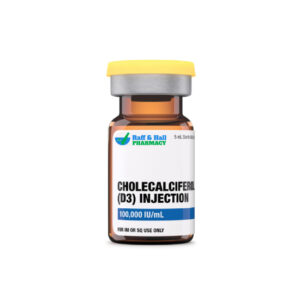
Two main forms of the fatsoluble vitamin D are cholecalciferol (vitamin D3) and ergocalciferol (vitamin D2). Ten times more powerful than ergocalciferol, cholecalciferol has a tenfold increase in effectiveness. It also triggers a faster serum calcidiol production response, which persists longer at higher levels. Fish liver oils, fatty fish, and eggs from hens supplemented with vitamin D are among other dietary sources.
After sunlight exposure, the skin produces cholecalciferol. In people without disease, 7dehydrocholesterol in the skin transforms into cholecalciferol. About 20% of body surface area to sunlight briefly exposure equals consuming 200 IU of cholecalciferol. Cutaneous production is therefore very effective. Many people, however, lack the capacity to effectively generate enough stores of cholecalciferol. Hence, cholecalciferol intake is absolutely necessary.
The chemical structure variations between the two forms of vitamin D have no impact on metabolism or clinical results once activated inside the body. While animal studies have revealed a variation in toxicity between vitamin D2 and vitamin D3, human studies have been inconclusive. Correct calcium and phosphate balance is dependent on vitamin D, which also promotes regular bone development and mineralization. Measurements of 25hydroxyvitamin D [25(OH)D] serum levels, which reflect all sources of vitamin D (such as sunlight and dietary or from supplements), can guide patient specific dosage. Though cholecalciferol is indicated for use in many illness conditions, its main purpose nowadays is for vitamin D supplementation as well as for rickets prevention and treatment.
Thus, because scientific evidence supporting claimed benefit(s) for nutraceuticals is not always available, they are not controlled under the same limitations as medications. Consumers should also be aware that nutraceuticals are not subject to strict quality control criteria, and great variation can be found in both their potency and their purity.
Clinically, cholecalciferol is comparable to ergocalciferol; thus, clinicians should also take contraindications and cautions for ergocalciferol into account when starting cholecalciferol therapy.
Hypercalcemia, hypervitaminosis D, and vitamin D hypersensitivity or hypersensitivity to any of the excipients in the preparation all preclude the usage of cholecalciferol. One causative element in babies of idiopathic hypercalcemia when vitamin D intake must be limited is hypersensitivity to vitamin D.
Patients with renal disease, particularly renal failure, could be at higher risk for vitamin D-induced hypercalcemia even with typical doses. Adequate supplementation and, in pediatric patients, correct development depend on close clinical monitoring. According to guidelines from the National Kidney Foundation, use of a vitamin D analog seems preferable in patients with stage 3 or greater kidney disease.
Patients with fat malabsorption caused by malabsorption syndrome, cystic fibrosis, Crohn’s disease, some types of hepatic illness, gall bladder disease or biliary tract disorder may need Greater doses of vitamin D brought about by reductions in intestinal absorption. Some patients taking concurrent medicines (e.g., some anticonvulsants) may also need larger dosages. In such situations, the prescription of active vitamin D analogs might be favored.
According to the FDA, ergocalciferol (Vitamin D2) falls under risk level C; therefore, dietary supplements of cholecalciferol should be treated similarly with regard to pregnancy. Adverse consequences have not been noted with the ordinary daily consumption of Vitamin D within the recommended dietary daily intakes for a pregnant woman. Animal reproduction studies have found fetal abnormalities in numerous species related to hypervitaminosis D; consequently, the use of vitamin D more than the advised Unless, in the opinion of the doctor, the possible advantages outweigh the dangers involved, dietary allowance during a typical pregnancy should be shunned. With a Tolerable Upper Intake Limit of 4000 International Units/day, vitamin D’s RDI during pregnancy is 600 International Units/day.
At levels near to the maternal serum concentration, the 25hydroxyvitamin D metabolite of vitamin D (cholecalciferol) is spread into human breast milk. Typical breast milk Concentrations (sans maternal supplementation) are inadequate to avoid vitamin D deficit in newborns only breastfed and without any further vitamin D supplementation. One major cause of rickets in babies—particularly those with dark complexion breastfed by mothers who are not vitamin D deficient—prolonged, exclusive breastfeeding of children lacking recommended supplementation is a strong culprit.
Taking cholecalciferol with other forms of vitamin D is not advised because it may increase the risk of side effects or toxicity. Like other vitamin D types, it can raise phosphorus levels in the blood, so using it with phosphorus supplements should be done carefully. Magnesium is often included in vitamin D and calcium products, but in people with kidney problems, combining magnesium and cholecalciferol can lead to harmful magnesium buildup. Calcium is usually paired with vitamin D to support bone health, but it can sometimes cause high calcium levels, which may lead to health problems. Long-term use of aluminum-based antacids along with vitamin D may result in aluminum toxicity, especially in those with kidney issues. Some seizure medications, like barbiturates or phenytoin, can interfere with vitamin D, potentially causing bone disorders, so careful monitoring and dosage adjustments might be needed. People with heart conditions or using certain heart medicines should use cholecalciferol with caution, as it may affect heart rhythms. Other medicines, such as certain diuretics or fat absorption blockers, can reduce how much vitamin D the body absorbs. Staggering the timing of these medications helps reduce interactions and maintain health.
Generally speaking, recommended dietary intakes of supplemental vitamin D do not cause any severe negative effects. Overdose of vitamin D may have adverse effects; yet, such symptoms connected with hypervitaminosis D (and the resulting hypercalcemia) are rarely reported. An overabundance of vitamin D results in excessively great calcium in the blood, which is almost always brought on by vitamin D analogs (e.g., calcitriol, doxercalciferol, paricalcitol) rather than the vitamin D present in nutritional supplements (e.g., cholecalciferol, ergocalciferol). But patients consuming greater vitamin D supplements should note any of the following possible indicators of high vitamin D/calcium levels: nausea/vomiting, constipation, loss of hunger, polydipsia, increased urinary frequency, mental/mood changes or irritation, headache, abnormal exhaustion or lethargy. These symptoms may need medical examination. Anorexia, weight loss, polyuria, and cardiac arrhythmia may also be seen. Furthermore, hypercalcemia from bone resorption causing hypercalciuria may be seen in prolonged hypervitaminosis D. Early signs of vitamin D poisoning include modest hypercalcemia and normal renal function. As vitamin D toxicity continues, increased calcium levels and ongoing bone resorption lead to suppression of parathyroid production. Calcification of the vasculature and other tissues long-term vitamin D toxicity has been linked with Has. Death from vitamin D is not backed by evidence linking it with kidney stones. Failure of the kidneys and cardiovascular systems probably accounts for D intoxication. Vitamin D toxicity results from long-term dosages of 10,000–40,000 International Units/day and long-term serum 25(OH)D levels of 500–600 nmol/L (200–400 ng/mL). Symptoms of vitamin D toxicity can become apparent within 4 weeks of constant, extreme consumption. Because vitamin D has a long halflife, symptoms of Toxicity might last a long time. High sun exposure does not cause vitamin D poisoning.
Risk of growth inhibition in infants caused by vitamin D supplementation is founded on a 1938 survey of 35 babies up to 45 weeks old. Age during which high-dose vitamin D supplements (1800 to 4500 IU daily for six months) were linked to growth inhibition as opposed to lower dose vitamin D supplements. (< 340 International Units daily for six months). In a following but smaller 1966 experiment (n = 11), vitamin D supplements showed no link to growth inhibition. Because of a potential relationship, no RDI for vitamin D for infants has been established.
FDA pregnancy risk group C describes ergocalciferol (Vitamin D2); dietary supplements of cholecalciferol should be handled likewise in reference to pregnancy. With the usual daily intake of Vitamin D within the advised dietary daily intakes for a pregnant woman, no adverse effects have been observed. Animal reproduction studies have shown fetal abnormalities in several species linked with hypervitaminosis D; hence, consumption of vitamin D beyond the recommended Unless, in the opinion of the doctor, the possible advantages outweigh the hazards involved, dietary allowance should be avoided during ordinary pregnancy. With a Tolerable Upper Intake Limit of 4000 International Units/day, the RDI of vitamin D during pregnancy is 600 International Units/day.
Regular breast milk Concentrations (without maternal supplementation) are not high enough to avoid vitamin D deficiency in babies only breastfed and who do not get other vitamin D supplementation. In darkskinned children breastfed by mothers who are not vitamin D sufficient, protracted, exclusive nursing of newborns without recommended supplementation is a major cause of rickets. Usually regarded as safe is vitamin D intake within the suggested daily diet for lactating women. While nursing, vitamin D’s recommended daily intake is 600 International Units/day with a Tolerable Upper Intake Limit of 4000 International Units/day. Highdose vitamin D supplementation for nursing mothers has been shown to boost 25(OH)D and vitamin D concentration in breast milk. Levels in babies: though the findings have not been confirmed, it is still advised to supplement to youngsters. Typically, the infant’s serum calcium levels should be monitored when a nursing mother is prescribed vitamin D in high doses as hypercalcemia has High dose maternal usage has been linked in reports.
Store this medication at 68°F to 77°F (20°C to 25°C) and away from heat, moisture and light. Keep all medicine out of the reach of children. Throw away any unused medicine after the beyond-use date. Do not flush unused medications or pour down a sink or drain.
- Nasim B, Al Sughaiver HMZ, Abdul Rahman SM, Inamdar RFB, Chakaki R, Abuhatab S. Efficacy of Vitamin D3 versus Vitamin D2 in Deficient and Insufficient Patients: An Open-Label, Randomized Controlled Trial. Ibnosina Journal of Medicine & Biomedical Sciences. 2019; 11(2): 57-61.
- Institute of Medicine (IOM), Food and Nutrition Board. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press, 2011.
- Drisdol (ergocalciferol) package insert. New York, NY: Sanofi-Synthelabo, Inc.; 2009 Nov.
- Kidney Disease Improving Global Outcomes. KDIGO Clinical Practice Guideline for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD_MBD). 2009. http://www.kdigo.org/pdf/KDIGO%20CKD-MBD%20GL%20KI%20Suppl%20113.pdf.– LinkOpens in New Tab
- Standing Committee on the Scientific Evaluation of Dietary Reference Intakes – Panel on Dietary Reference Intakes, Food and Nutrition Board, Institute of Medicine (IOM). Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. The National Academy of Sciences Press, Washington DC; 1997
- Wagner CL, Greer FR, and the Section on Breastfeeding and Committee on Nutrition. Prevention of rickets and Vitamin D deficiency in Infants, Children, and Adolescents. Pediatrics 2008;112:1142-1152.
- Rocaltrol® (calcitriol) package insert. Nutley, NJ: Roche Laboratories, Inc.; 2004 Jul.[/fn][fn]Hectorol® (doxercalciferol) package insert. Middleton, WI: Bone Care International, Inc.; 2005 Jun.
- Hectorol® (doxercalciferol) package insert. Middleton, WI: Bone Care International, Inc.; 2005 Jun.
- Chan JC, Jacob M, Brown S, et al. Aluminum metabolism in rats: effects of vitamin D, dihydrotachysterol, 1,25-dihydroxyvitamin D and phosphate binders. Nephron1988;48:61—4.
- McNamara JO. Drugs effective in the therapy of the epilepsies. Gilman AG, Hardman JG, Limbird LE, (eds.) In: Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 10th ed., New York, McGraw-Hill Companies. 2001:530—2.
- Marcus R. Agents affecting calcification and bone turnover: Calcium phosphate, parathyroid hormone, vitamin D, calcitonin, and other compounds. Gilman AG, Hardman JG, Limbird LE, (eds.) In: Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 10th ed., New York, McGraw-Hill Companies. 2001:1715—43.
- Lanoxin® (digoxin) package insert. Research Triangle Park, NC: Glaxo Smith Kline; 2001 Aug.
- Amin S, LaValley MP, Simms RW, et al. The role of vitamin D in corticosteroid-induced osteoporosis: an analytical approach. Arthritis Rheum 1999;42:1740—51.
- Reid IR. Preventing glucocorticoid-induced osteoporosis. N Engl J Med 1997;337:420—1.
- Questran® and Questran® Light (cholestyramine) package insert. Spring Valley, NY: Par Pharmaceutical Inc; 2002 July.
- Xenical® (orlistat) package insert. Nutley, NJ: Roche Laboratories Inc.; 2005 Jan.
- Hypponen E, Fararouei M, Sovio U, et al. High-dose vitamin D supplements are not associated with linear growth in a large Finnish cohort. J Nutr 2011;141:843-848.